Changing perceptions
about
the categorization of ALS
Historically, patients with ALS were categorized in 1 of 2 groups: those with familial ALS (fALS), which is inherited from a family member, and those with sporadic ALS (sALS), which occurs without a known family history of the disease.1 But now there is a new way of looking at ALS.
Genetic ALS / Redefining sALS and fALS
What constitutes familial ALS (fALS) and sporadic ALS (sALS)?
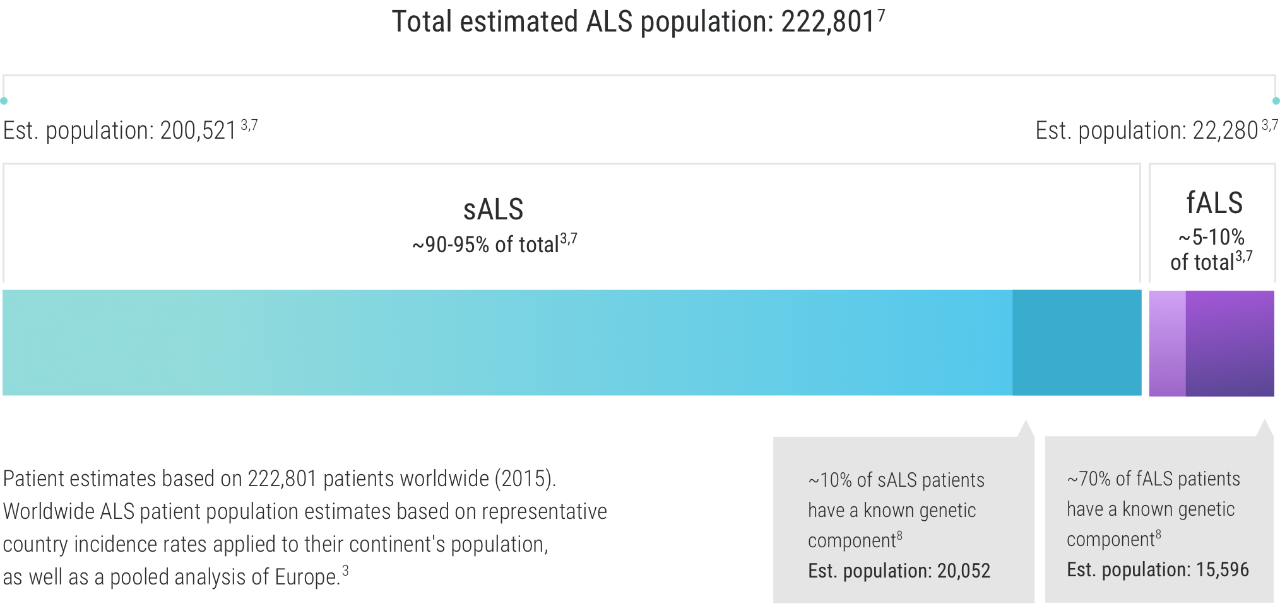
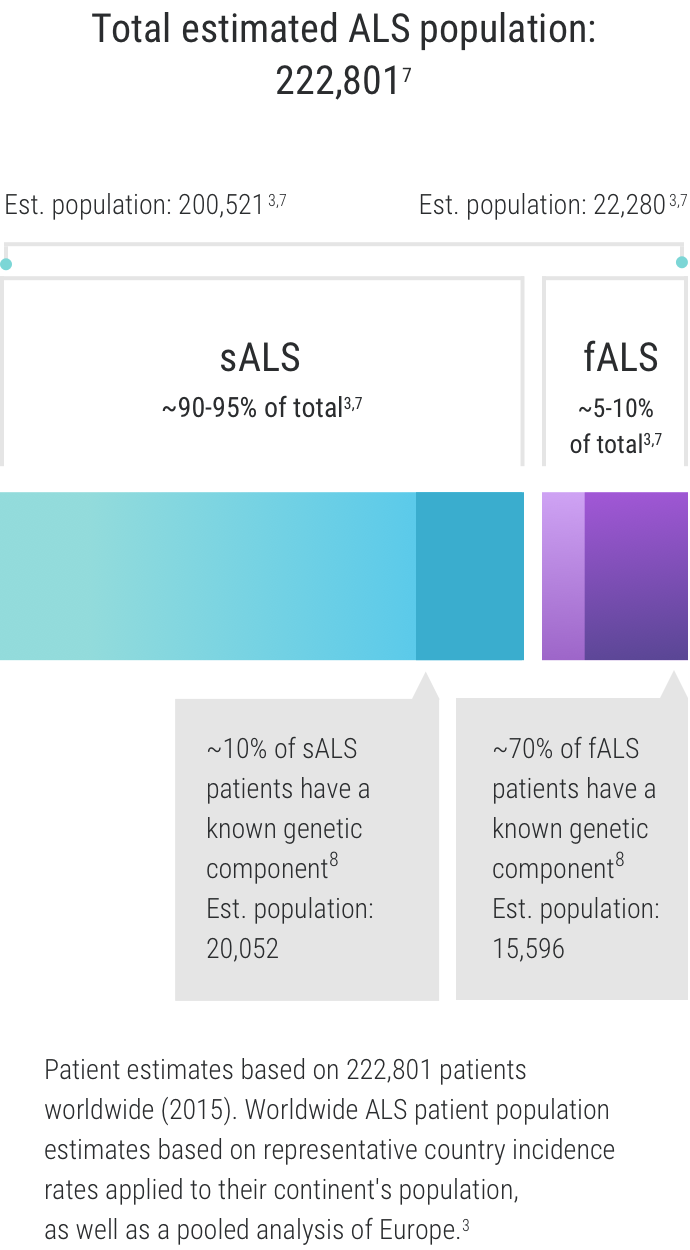
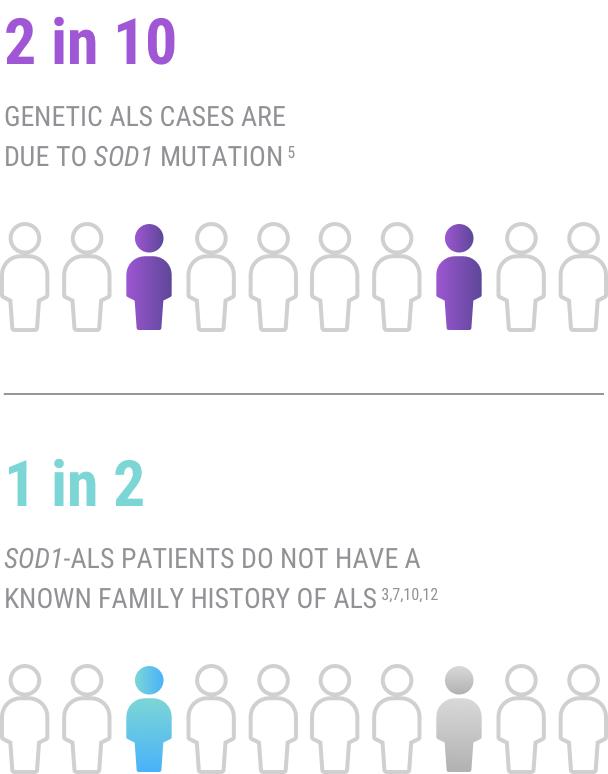
Approximately 5%-10% of all patients with ALS are thought to have fALS, while sALS accounts for about 90-95% of all ALS cases.1-3 There is now a deeper understanding of the role of genetics in ALS, which has provided new insights into the categorization of ALS. When referring to “genetic ALS,” we are not only referring to familial ALS. Recent discoveries showed that those diagnosed with both familial and sporadic ALS have a genetic component to their disease. This has led to a deeper understanding of the disease—and new insights for researchers.3-6
There is no clear pathologic mechanism that can be ascribed to the development of ALS, but experts believe that an interaction among genetic, epigenetic, and environmental factors may play a role.5,9
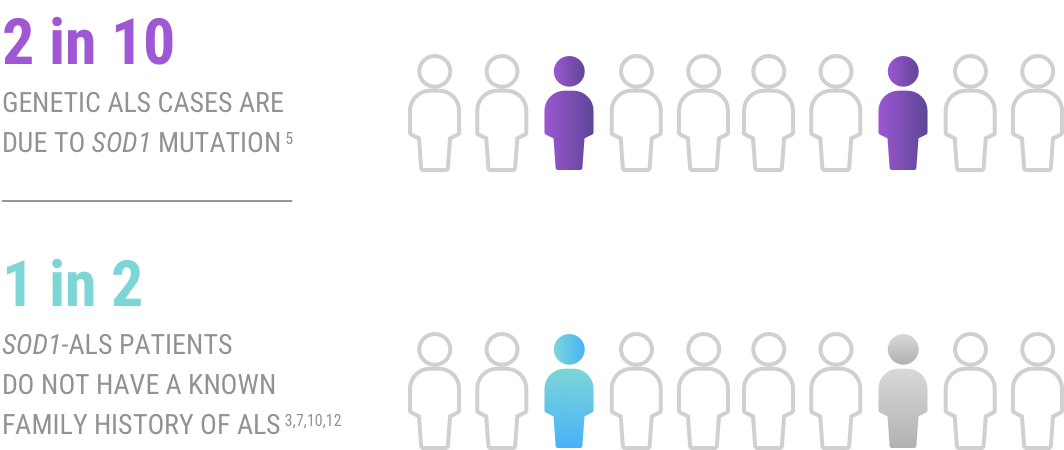
While it may seem that a genetic association with ALS would only be found in patients with fALS since genetic mutations are inherited from one’s parents, this is not the case. This means that even if a patient has no known family history of ALS, a genetic component may still be involved.2
Prof. Albert Ludolph
University Hospital in Ulm, Germany
“We still use the terms ‘familial ALS’ and ‘sporadic ALS’ to refer to the patients we treat. But that’s mainly because the terms are recognized; they’ve become shorthand. In reality, we know that a large portion of ALS risk is genetic, and many patients previously considered to have a ‘sporadic’ form of the disease carry potentially pathogenic mutations.10,11 There was a time when we did not do a gene panel for all of our ‘sporadic’ patients, but that has changed. We have now established a genetic panel for all of our patients. We are currently sequencing 2,500 of them.” says Prof. Ludolph.
Genetic testing in patients with sporadic ALS
Because a number of gene mutations have been found in patients with both fALS and sALS, a genetic test may be considered for anyone with an ALS diagnosis.5 Even though the percentage of sALS cases with a genetic component is smaller than that for fALS cases (approximately 10% of sALS cases compared to ~70% of fALS cases), their total number may account for the majority of ALS cases associated with a genetic mutation. This is because sALS cases make up about 90-95% of all ALS cases.1-3
Genetic testing for all ALS patients may also help provide a better understanding of the basis of their condition, allowing for more informed healthcare decisions and life choices.
Clinical trials for genetic ALS are currently enrolling patients with specific mutations—another reason to discover which ALS-associated mutations a patient may have.5,13
“Our focus now is on performing genetic testing in families with autosomal dominant traits. We have 500 of these families in Germany right now. There was a time when we did not do sequencing or genetic testing for all our sporadic patients. This has begun to change.”
– Prof. Albert Ludolph
References: 1. Brown RH, Al-Chalabi A. Amyotrophic Lateral Sclerosis. N Engl J Med. 2017;377(2):162-172. 2. Nguyen HP, Van Broeckhoven C, van der Zee J. ALS genes in the genomic era and their implications for FTD. Trends Genet. 2018;34(6):404-423. 3. Zarei S, Carr K, Reiley L, et al. A comprehensive review of amyotrophic lateral sclerosis. Surg Neurol Int. 2015;6:171. doi:10.4103/2152-7806.169561 4. Byrne S, Walsh C, Lynch C, et al. Rate of familial amyotrophic lateral sclerosis: a systemic review and meta-analysis. J Neurol Neurosurg Psychiatry. 2011;82:623-627. 5. Roggenbuck J, Quick A, Kolb SJ. Genetic testing and genetic counseling for amyotrophic lateral sclerosis: an update for clinicians. Genet Med. 2017;19(3):267-274. 6. Renton AE, Chiò A, Traynor BJ. State of play in amyotrophic lateral sclerosis genetics. Nat Neurosci. 2014;17(1):17-23. 7. Arthur KC, Calvo A, Price TR, Geiger JT, Chiò A, Traynor BJ. Projected increase in amyotrophic lateral sclerosis from 2015 to 2040. Nat Commun. 2016;7:12408. doi:10.1038/ncomms12408 8. Volk E, Weishaupt JH, Andersen PM, Ludolph AC, Kubisch C. Current knowledge, and recent insights into the genetic basis of amyotrophic lateral sclerosis. Med Genet. 2018;30(2):252-258. 9. Vucic S, Higashihara M, Sobue G, et al. ALS is a multistep process in South Korean, Japanese, and Australian patients. Neurology. 2020;94(15):e1657-1663. 10. Chiò A, Mazzini L, D’Alfonso S, et al. The multistep hypothesis of ALS revisited: the role of genetic mutations. Neurology. 2018;91(7):e635-e642. doi:10.1212/WNL.0000000000005996 11. Shepheard SR, Parker MD, Cooper-Knock J, et al; on behalf of Project MINE Consortium; Project MinE. Value of systematic genetic screening of patients with amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry. 2021;92(5):510-518. 12. Lattante S, Marangi G, Doronzio PN, et al. High-throughput genetic testing in ALS; the challenging path of variant classification considering the ACMG guidelines. Genes. 2020;11:1123. 13. Benatar M, Stanislaw C, Reyes E, et al. Presymptomatic ALS genetic counseling and testing: experience and recommendations. Neurology. 2016;86(24):2295–2302.
1. Brown RH, Al-Chalabi A. Amyotrophic Lateral Sclerosis. N Engl J Med. 2017;377(2):162-172. 2. Nguyen HP, Van Broeckhoven C, van der Zee J. ALS genes in the genomic era and their implications for FTD. Trends Genet. 2018;34(6):404-423. 3. Zarei S, Carr K, Reiley L, et al. A comprehensive review of amyotrophic lateral sclerosis. Surg Neurol Int. 2015;6:171. doi:10.4103/2152-7806.169561 4. Byrne S, Walsh C, Lynch C, et al. Rate of familial amyotrophic lateral sclerosis: a systemic review and meta-analysis. J Neurol Neurosurg Psychiatry. 2011;82:623-627. 5. Roggenbuck J, Quick A, Kolb SJ. Genetic testing and genetic counseling for amyotrophic lateral sclerosis: an update for clinicians. Genet Med. 2017;19(3):267-274. 6. Renton AE, Chiò A, Traynor BJ. State of play in amyotrophic lateral sclerosis genetics. Nat Neurosci. 2014;17(1):17-23. 7. Arthur KC, Calvo A, Price TR, Geiger JT, Chiò A, Traynor BJ. Projected increase in amyotrophic lateral sclerosis from 2015 to 2040. Nat Commun. 2016;7:12408. doi:10.1038/ncomms12408 8. Volk E, Weishaupt JH, Andersen PM, Ludolph AC, Kubisch C. Current knowledge, and recent insights into the genetic basis of amyotrophic lateral sclerosis. Med Genet. 2018;30(2):252-258. 9. Vucic S, Higashihara M, Sobue G, et al. ALS is a multistep process in South Korean, Japanese, and Australian patients. Neurology. 2020;94(15):e1657-1663. 10. Chiò A, Mazzini L, D’Alfonso S, et al. The multistep hypothesis of ALS revisited: the role of genetic mutations. Neurology. 2018;91(7):e635-e642. doi:10.1212/WNL.0000000000005996 11. Shepheard SR, Parker MD, Cooper-Knock J, et al; on behalf of Project MINE Consortium; Project MinE. Value of systematic genetic screening of patients with amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry. 2021;92(5):510-518. 12. Lattante S, Marangi G, Doronzio PN, et al. High-throughput genetic testing in ALS; the challenging path of variant classification considering the ACMG guidelines. Genes. 2020;11:1123. 13. Benatar M, Stanislaw C, Reyes E, et al. Presymptomatic ALS genetic counseling and testing: experience and recommendations. Neurology. 2016;86(24):2295–2302.